The Royal College of Emergency Medicine (RCEM) has just published a four-page document called The Roadmap to Recovery.
It contains four sets of recommendations for improving the quality of care in emergency departments in the UK, but here I want to concentrate on the first of them: End overcrowding in Emergency Departments and ambulance queues outside of hospitals.The recommendation made by the RCEM that I want to focus on is this one: "Ensure that there are enough hospital beds available that are appropriately staffed, so hospitals have the space and resources available to be able to care for all the patients who need emergency admission."
I totally, vehemently agree with this recommendation.
But I also have a problem with it, which is that it is too 'over-arching'. If we want to improve a hospital's patient flow, there's no point saying over-arching things like "Ensure that there are enough hospital beds available ... so hospitals have the space and resources available to be able to care for all the patients who need emergency admission.". No. Sorry. Too vague. We need instead to be saying specialty-specific things like for example: "Respiratory Medicine in Hospital X needs to reduce its bed occupancy from 110% to 91%, and we think the best way of doing that is to reduce its admissions from 7.5 per day to 7.1 per day and reduce its mean length of stay from 6.75 days down to 5.9 days.
Why this obsession with specificity? Am I just reacting like a typical detail-obsessed data nerd, concerned only about describing complex reality when I should instead be making generalizations in an attempt at improving reality?
Well, in a way, yes. And it's deeply unfair of me to criticize a UK-wide body like the RCEM for not being specific. I get that. But the problem is that it's not just UK-wide bodies that fail to get specific. Even individual hospitals fail to get specific. Everyone has this tendency to think about a hospital's inpatient beds as if they were a single, amorphous entity. But they're not. Hospital beds are highly differentiated entities. They need to be carefully disaggregated into their individual component specialties and described with their own specialty-specific numbers and dynamics.
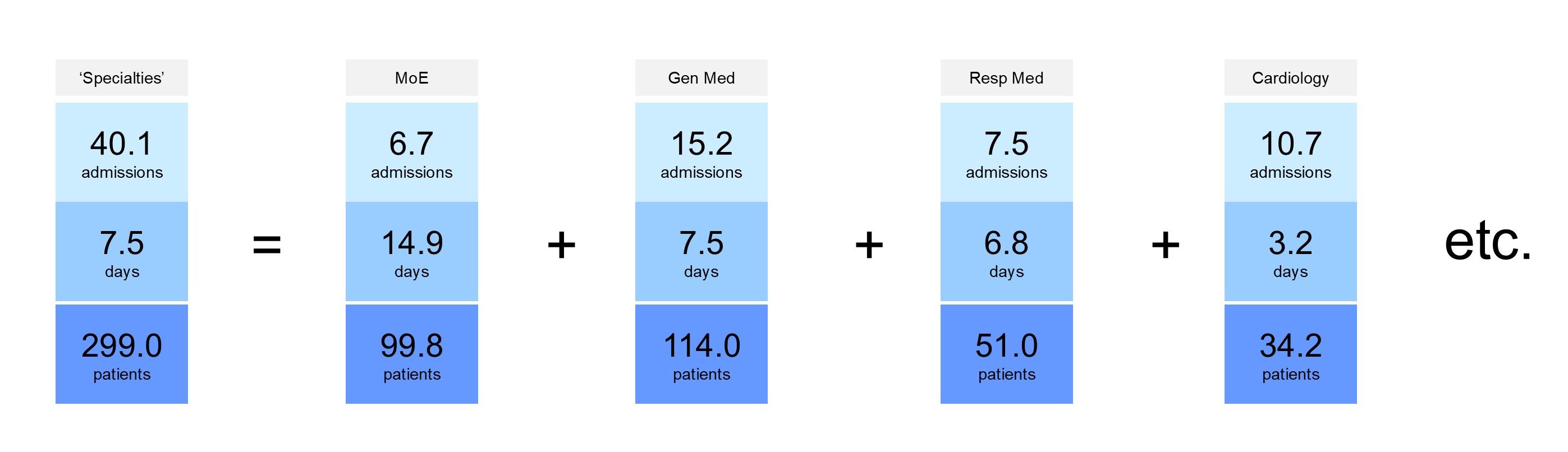
I cannot stress this enough. I think there's a tendency for national bodies to just assume that down at operational level, down at the coalface, of course individual specialties must be closely monitoring their flow metrics—their inpatient admissions, their length of stay, their bed occupancy—on a routine basis. In fact, I think there's even a tendency for trust board-level bodies to assume that hospital inpatient specialties are given these indicators and that they keep a close eye on them.
But I don't think that is actually the case.
And even if it is, then I'm not sure that the mechanism by which these flow performance indicators are delivered to the inpatient specialties is the right one. My anxiety is that the indicators might be there, somewhere, but they'll be tucked away on some obscure, out-of-the-way dashboard, in a tiny, barely-legible typeface so that—in reality—nobody actually bothers looking at them.
It's interesting that, towards the end of the RCEM's paper, there's a bit about information. It says: "Meaningful performance information supports the NHS to improve the quality and safety of care" but it doesn't say anything about the fact that there may actually be a performance information black hole at exactly the point in the system (the inpatient specialties) where it might have the most impact on emergency department crowding.
Acute hospitals need to make available to each specialty its indicators. Its actual numbers, its 'ought-to-be' numbers. The specialties need to have routine meetings at which these numbers are presented and discussed. Moreover, we shouldn't just be showing each specialty their own numbers; we should be enabling every specialty to see everyone else's numbers, too. Let everyone see everything. Avoid the silo mentality. Create some sort of collective accountability, some sense of joint endeavour.
My theory why this doesn't happen already is that too many people assume—incorrectly—that the individual specialties can access these numbers already, but that they're powerless to change them. Well, maybe the second part of that sentence is true, but I'm pretty sure the first part isn't. And even if hospitals do publish individal specialties' flow metrics, they're probably not counting them properly and they're probably not publishing them in a forum where they can debated, discussed and acted on.
[26 August 2024]