Two months ago, the Health Foundation published a thought paper called Understanding analytical capability in health care. The first paragraph of the report sets out the problem it was addressing:
People that are able to manipulate, analyse and interpret data are essential for a modern health care system. But there is an acknowledged problem that health services in the UK often cannot access the right level of skilled analysts and data scientists to support decision making. This deficit exists across all sectors and levels within health care. Therefore it is important that, in addition to strategies for investment in new information technology and big data, the data analysis workforce is also considered.
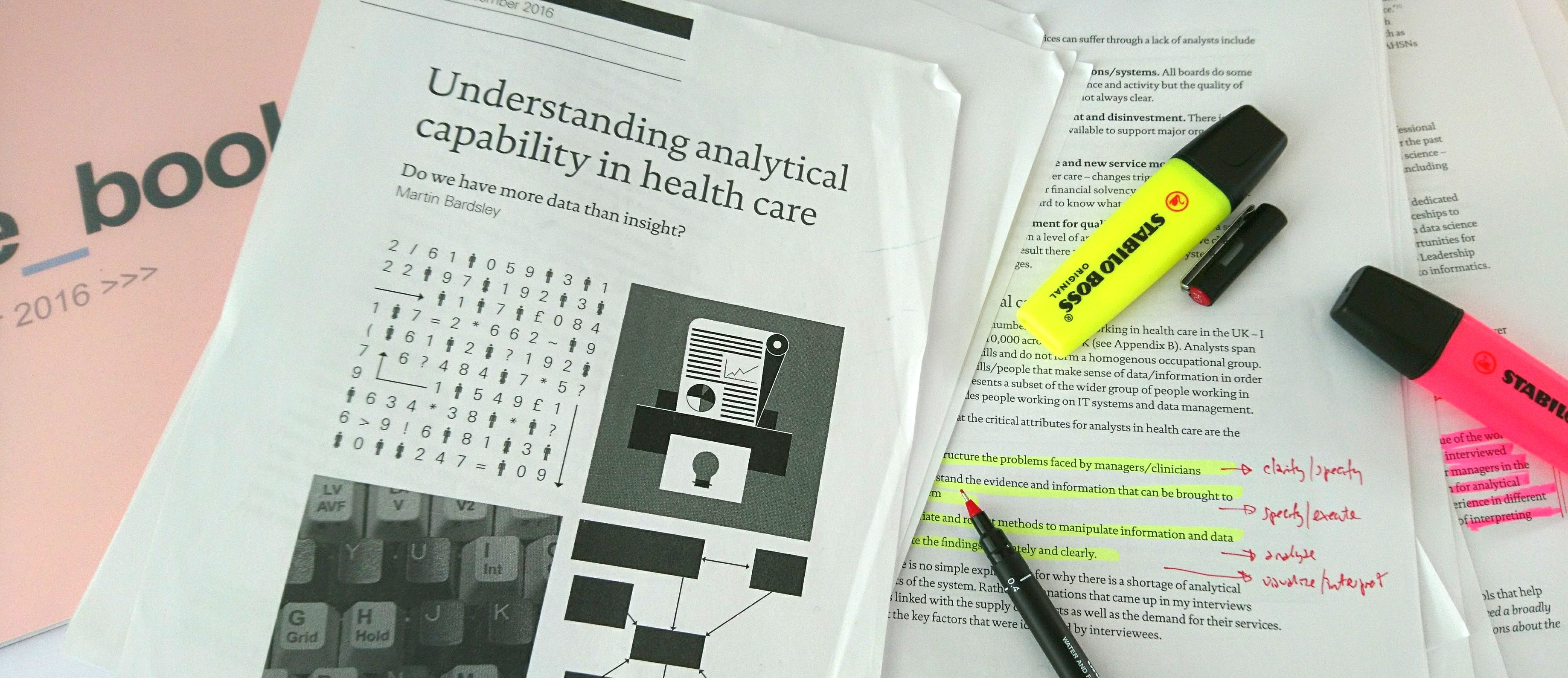
One of the things I particularly like about this excellent paper (and which I want to focus on here) is its definition of what constitutes data analysis in healthcare. It's a broad-based definition, and it contains four elements. I'm quoting from page four of the report here (although these attributes are mentioned again on page 13):
The critical attributes of analysts in health care are the ability to:
1. Understand and structure the problems faced by managers/clinicians
2. Access and understand the evidence and information that can be brought to bear on a problem
3. Apply appropriate and robust methods to manipulate information and data
4. Communicate the findings accurately and clearly
In my experience the middle two of these attributes are universally accepted as necessary attributes; the two outer ones (understanding managers' problems and communicating information clearly) are, however, less generally acknowledged.
One way of characterising the difference between the two inner attributes and the two outer attributes is to say that the two inner ones are data-facing attributes, whilst the two outer ones are manager-facing attributes. You can access data and analyse data on your own. You just need a computer. But understanding problems and communicating findings cannot usually be done unless decision-makers are present. The two outer attributes are about engagement.
So when—towards the end of the report—we see some recommendations of the types of training and development intervention that might help with solving the problem of analytical capability in health care, I started to think about the possibilities of interventions that were aimed at both analysts and managers together.
My emerging view is that the focus of these things in terms of training and development needs to be on a joint, multi-disciplinary approach. Analysts need to be in the same room as managers when we try to improve analytical capability in health care.
Why?
Three reasons.
Firstly, the paper suggests that we need to grow and develop informatics leaders in the NHS. Leaders are "that tribe of people who understand the possibilities of good analysis yet can also engage with managers at the highest levels to influence and shape demand." So if these attributes why not involve both tribes in the training and development process itself?
Secondly, the paper makes several mentions of the need for networks for analysts to work in and be a part of. And usually what we mean by networks is networks of information analysts, and yes, we desperately need those, but—in the absence of that, and while we're working on how to improve that—why not create our own communities of practice within our own organisations but define the practice more broadly, so that it encompasses the specification, the use and the interpretation of data as well as the more conventionally "core" data tasks. One way to encourage data analysts to be manager-facing and decision-facing might be to find a way of encouraging us to make these networking links at local level.
Thirdly, the paper makes a strong point (on page 32) about how analytics as a profession needs to get better at demonstrating business benefit if it is to be taken more seriously and given the higher profile we want for it. And it strikes me that if this is a key outcome of what we are trying to do, then we should try to design our training and development interventions around examples of how data can be brought to bear on decision-making and how communication and collaboration between analysts and managers is done in practice.
Nick Tordoff and I have been developing this collaboration-based approach to informatics training over the last two-and-a-half years as part of the East Midlands Academic Health Science Network's Information Analyst Development Programme. We jointly designed a one-day workshop-called Data Conversations that is explicitly aimed at a multi-disciplinary audience: analysts, managers and clinicians.
But we need more of this kind of thing. Information that supports decision-making in the NHS is too important to be left just in the hands of information analysts. If we are serious about improving analytical capability, we need to be doing this together with managers and clinicians. All of us in the same room.
[17 February 2017]