Flow_ology is a one-day course for data analysts who have a familiarity with acute hospital unscheduled care data. The course proposes a way of analysing and presenting data that will help managers and clinicians understand and improve patient flow. The course assumes that analysts will need to present data on patient flow to four types of meeting, and each 90-minute session is devoted to preparing the data exhibits for each meeting.
Session 1
9:30 to 10:45
Establish the mental model of patient flow
We visualize patient flow in acute hospitals as the movement of patients through a series of staging posts. Most unscheduled care patients present first at the emergency department. Then a proportion of them move to either an admissions ward (for example, an acute medical unit) or a specialty ward. Within these three staging posts, we need to measure three flow metrics: (1) how many; (2) how long and (3) how full. With the three staging posts as columns and the three flow metrics as rows, we arrive at our mental model as a 3 x 3 grid. And the key thing we have to do with this grid is split it into two grids. One on the left looks at the best patient flow days of the year; the one on the right looks at the worst patient flow days of the year.
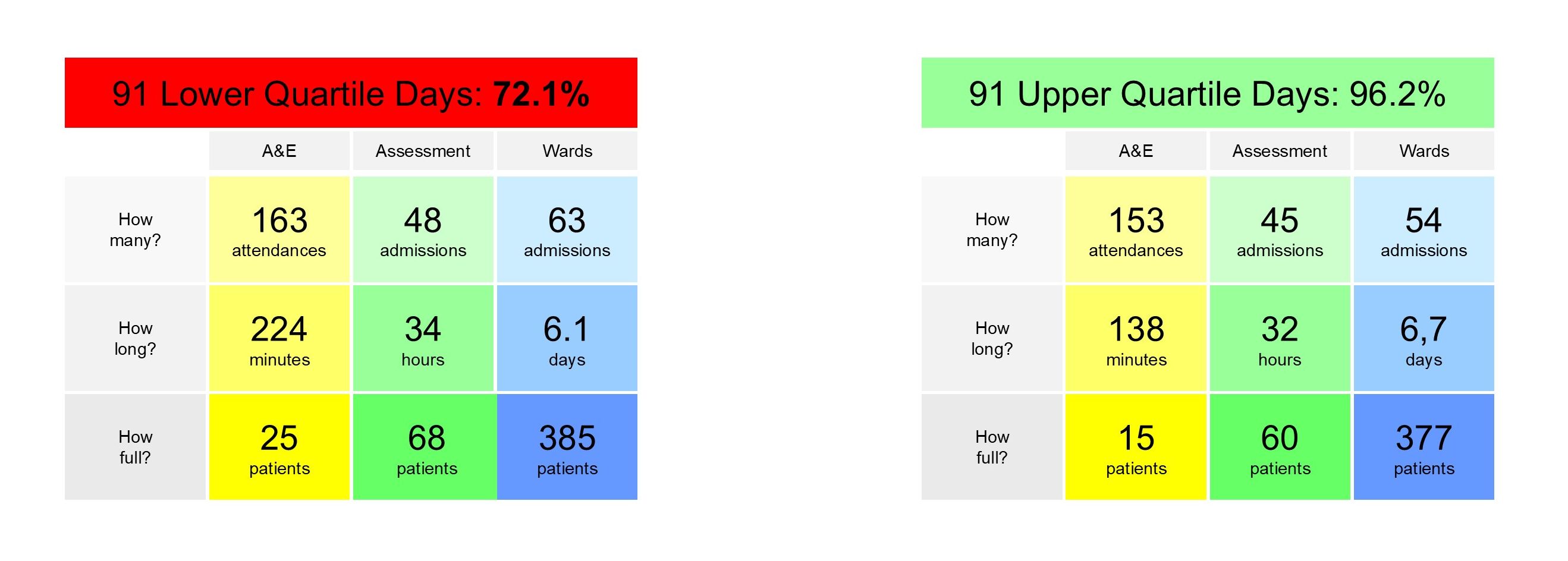
The grids aren't just sets of nine numbers; they are a way of understanding how the staging posts interact with each other. We need to understand the cause-and-effect relationships between the numbers in the grid, and then combine that knowledge with Little's Law arithmetic in order to arrive at 'ought-to-be' numbers for the different parts—clinical specialties—of the system.
Session 2
11:15 to 12:45
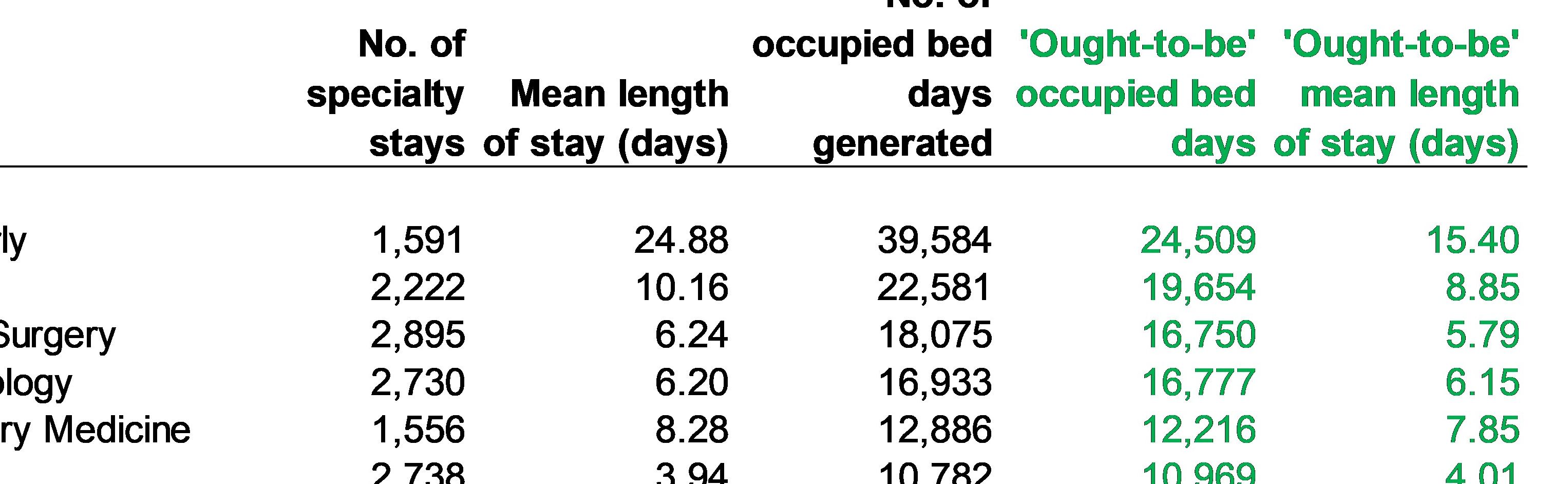
Work out the top-level 'ought-to-be' numbers
Once we've gained the 'analytical self-confidence' that stems from an understanding of the cause-and-effect relationships, we can set about the task of working out the levels of fullness, length of stay and activity that the hospital should be working towards if it is to improve patient flow. These top-level numbers will be presented to the senior management level at the hospital. We may need to do more than one of these meetings, but the emphasis at this stage will be on the top-level numbers for the hospital as whole, even though those numbers have been arrived at by means of a specialty-by-specialty 'bottom-up' process.
Session 3
13:30 to 14:45
Present the 'ought-to-be' numbers
The next level of meetings we need to prepare for are the individual clinical directorate meetings. Each directorate needs its own meeting, so this level could involve up to 15-20 meetings, depending on the number of individual specialties. The data we need to present to these meetings needs to be more detailed. We need to demonstrate that we understand all the nuances of the data at specialty level. For example: what happens when patients transfer in and out of critical care wards? What use does a specialty make of 24-hour day case facilities?
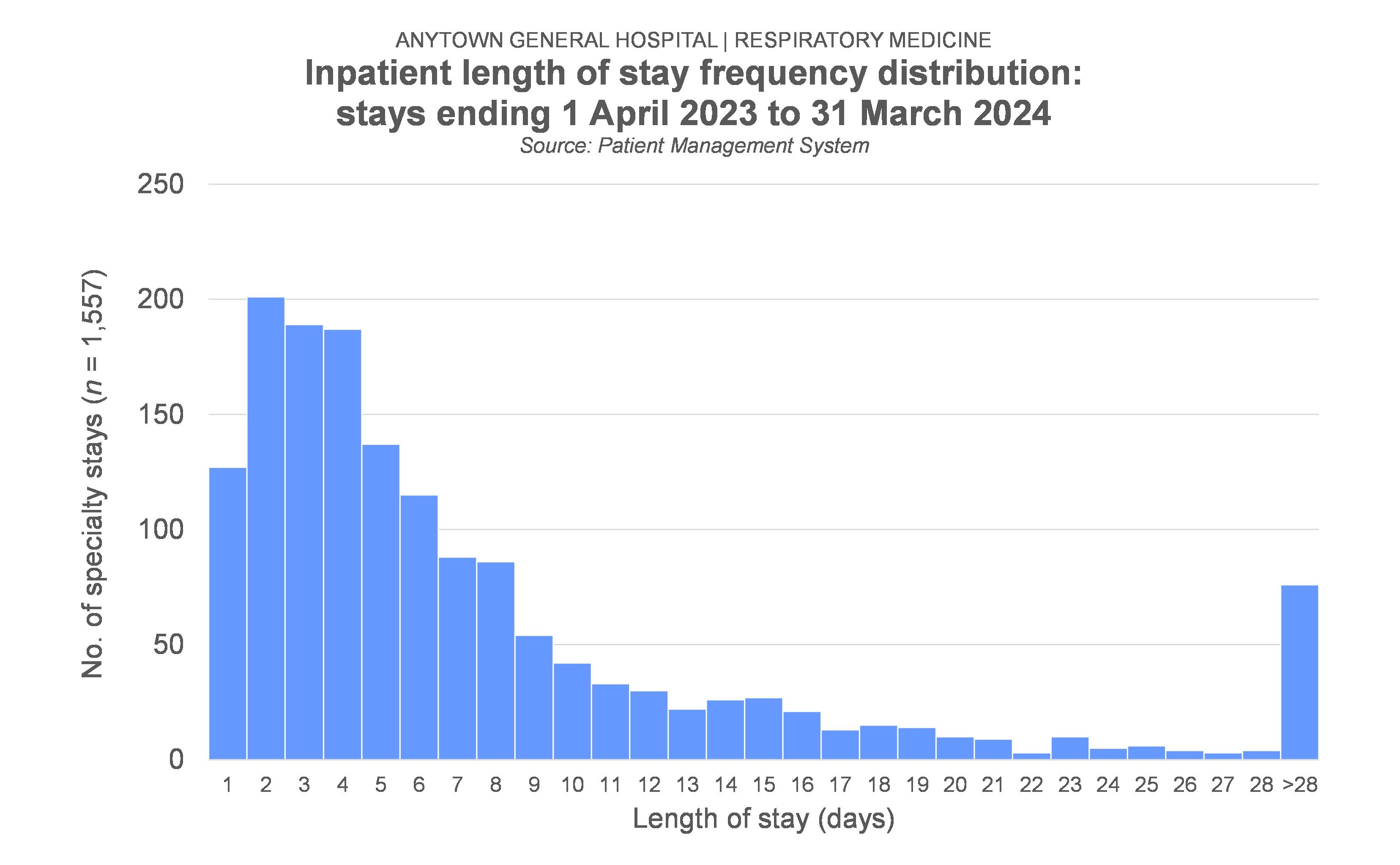
But our objective with these directorate-level meetings is not just to show that we've got the data (including the 'ought-to-be' numbers) right; we also want to show what length of stay looks like when we put it under the microscope. We'll be looking at length of stay histograms in some detail, and putting forward some modelled versions of what length of stay histograms ought to look like, and therefore what the impact on the specialty's bed occupancy might be if a new length of stay profile were to be adopted.
Session 4
15:00 to 16:15
Monitor the change
The meetings with the clinical directorate management teams will have given us permission to approach the individual medical and nursing staff in each directorate. Ideally, we want to be attending—and presenting data at—monthly meetings of these directorates from now on, so that we can monitor any progress that is being made towards the ought to be numbers. It's not enough to just show the data for that part of the system; we also have to keep providing directorates with a strong sense of context. They need to be able to see what is happening in other parts of the system, too.
Flow_ology can be booked as an on-site workshop for £1,250+VAT, and up to 12 participants can be accommodated in each workshop session. Email info@kurtosis.co.uk to start making arrangements.
Familiarity with Microsoft Excel and Microsoft PowerPoint is necessary for this training course.