Here is a sentence from the keynote speech Amanda Pritchard made yesterday to the NHS Confed Expo conference:
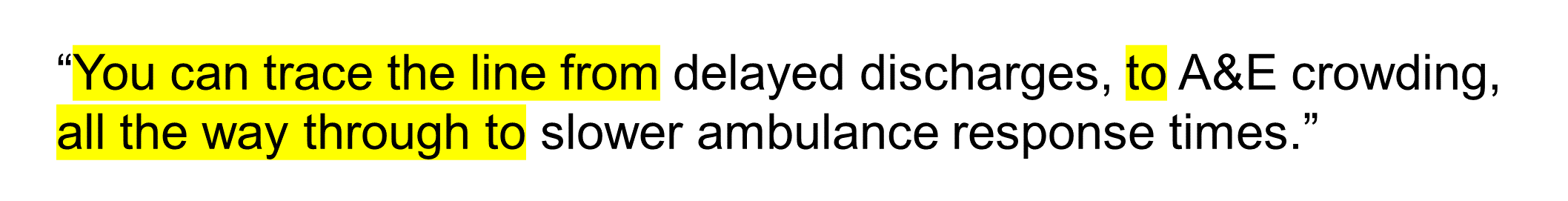
The thing I like about this sentence is that it describes the unscheduled care patient flow problem on two levels. First, there's the whole system level, shown by the words highlighted in yellow:
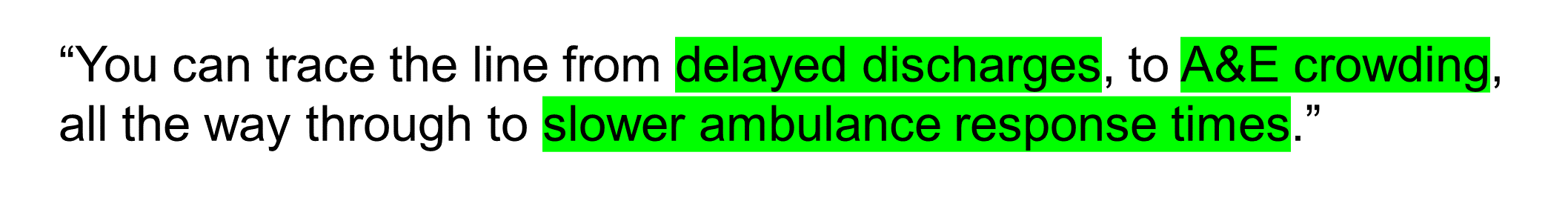
And then there is also what I want to call the exit block level, shown by the words highlighted in green:
Let's start with the exit block level.
It's important for us to understand exit block if we are to get our heads round patient flow. Exit block happens when you spend longer in a place because the next place you're going to doesn't have room for you. This happens at all stages in the unscheduled care system but the phrase tends to be mostly used to refer to the exit block experienced by Emergency Department (ED) patients. The admission wards they need to be transferred to are full and patients therefore have to wait for empty beds to become available.
At the other end of the spectrum of 'things we need to understand if we are to get our heads round patient flow' is the whole system idea. Things that happen in one part of the system have effects on other parts of the system. And usually it's not just straightforward cause-and-effect stuff; it can a lot more nuanced and multi-factorial. Just to keep us on our toes.
There is a bit of whole system thinking going on when we look at exit block. We have to connect two silos together (usually the ED and the admissions wards that are the next port of call) to make sense of exit block. But there's also this sense that there's more to the whole system than just the ED and the admissions wards; we have many more silos to consider and to connect to these two.
And yet—despite the fact that most of us seem to agree with the existence of these two levels (I have yet to come across 'exit block deniers' or 'whole system deniers'!)—Amanda Pritchard's sentence highlights for me that fact that actually we are pretty bad at joining these two approaches up in any sort of systematic way.
It's no good just saying "We need to do something about exit block in the Emergency Department" or "Of course, it's a whole system problem and unless we tackle the issues in social care we won't crack this". All of the different silos in between the Emergency Department and social care services have to be joined together, quantified systematically, and the cause-and-effect dynamics that connect them need to be described as precisely as we can. And we have to learn the habit of looking at all of these silos simultaneously, so that we can see how the cause-and-effect mechanisms between the silos actually work.
We have to join these two levels together. We need a 'bottom-up' approach that tackles each of the individual exit blocks in turn. And we also need the overall whole system approach that puts everything into one big picture.
And I think we can do this by being a bit more rigorous about the way we describe exit block.
Instead of just focusing on the traditional location of exit block: the ED and the (full) admissions wards, we need instead to focus on all the exit blocks, tackling them in order and simultaneously. We can start—for example—at the right-hand end of Amanda Pritchard's sentence (slower ambulance times), and we can look at the exit block experienced by ambulance crews trying to drop off patients at the Emergency Department.
Then we can move on to the 'original' exit block—the one that's the principal cause of the middle part of Amanda Pritchard's sentence—the A&E crowding—and look at how full the AMUs and the surgical assessment wards and the Orthopaedics Trauma wards are.
But then we have to look at the next exit block, the one that in my experience gets the least amount of attention: the specialty wards downstream of the admissions wards create exit block for the admissions wards. We absolutely need to start applying more attention to this transition, breaking down each of the downstream specialty areas into meaningful directorate-type chunks and identifying the 'ought-to-be' bed occupancies and lengths of stay that will help ensure flow in these specialty ward areas.
And then finally to the exit block at the left hand end of Amanda Pritchard's sentence: the delayed discharges. The exit block caused by delays in transferring patients to other hospitals, to care homes and—probably most pertinently—overstretched care at home services.
But we can't just look at one exit block without also looking at the other exit blocks. And we can't look at all of the exit blocks without making a concerted attempt to join them all together into a 'whole system' whole so that they make sense.
I tweeted on Thursday morning—in response to Amanda Pritchard's speech—that "Me, I want to paint that line with a brush so wide you'll be able to see it from Space!"
And the wide brush I'm starting to use is an approach that emphasises patient stories as opposed to tables and graphs.
FlowStories is an approach to the data on patient flow that restores its relevance and credibility. There is an open workshop in central London scheduled for Wednesday 20th July 2022. More details on the FlowStories webpage.
[16 June 2022]
If you want to get notifications by email of new content on the Kurtosis website, please just contact info@kurtosis.co.uk and ask to be added to the email subscription list.